By Alana Mauger
Monday, June 19th is an important day for celebration and awareness. It marks Juneteenth, our newest federal holiday and a day of reflection and pride that commemorates the ending of slavery in the United States.
It’s also World Sickle Day, established by the United Nations in 2008 and commemorated every June 19th to increase awareness about sickle cell disease – the most common genetic disorder in the U.S. An estimated 100,000 people in the U.S. are living with sickle cell disease, most of whom are of African or Latino descent.
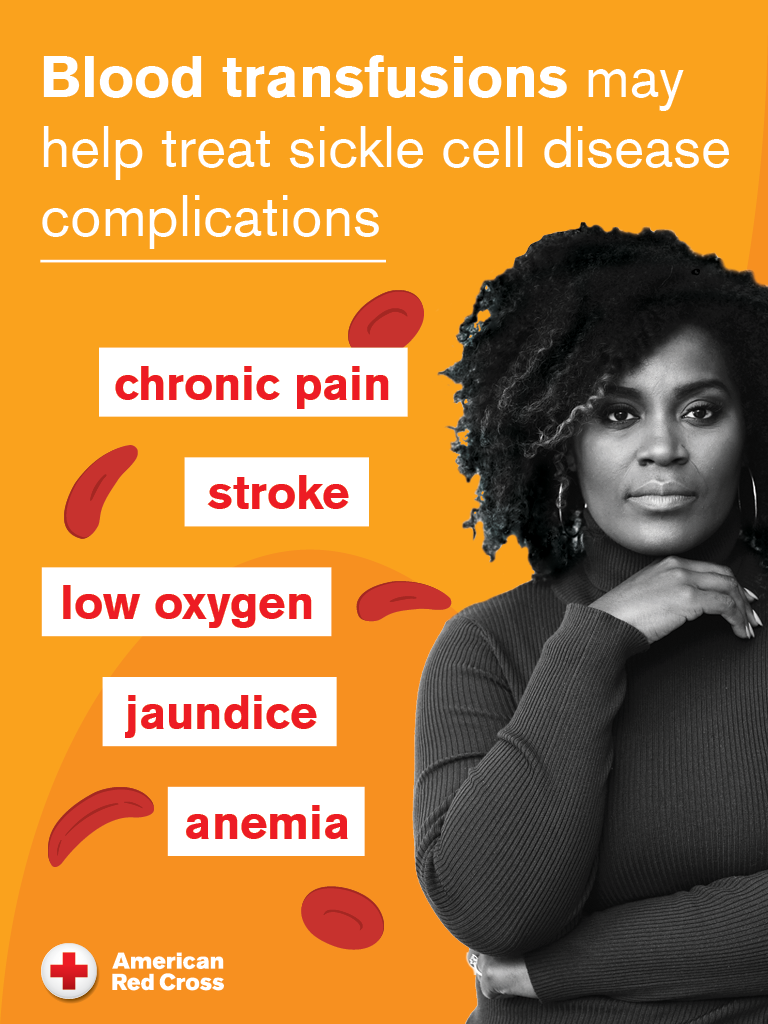
Sickle cell disease causes red blood cells to be hard and crescent-shaped – like a sickle – instead of soft and round, making it difficult for blood to flow smoothly and carry oxygen adequately to the rest of the body. Sickle cell warriors can experience complications like severe pain, anemia, infections, stroke and organ damage.
Blood transfusions help relieve sickle cell disease symptoms by increasing the number of healthy red blood cells in the body, helping to deliver oxygen throughout the body and unblocking blood vessels. But ensuring hospitals have an adequate supply of the major blood types – O, A, B and AB – is only part of the equation.
There are more than 600 known antigens – substances on red blood cells that help determine your blood type – some of which are unique to specific racial and ethnic groups. Individuals who require regular blood transfusions, like those with sickle cell disease, need blood that is matched more closely to reduce possible complications. Therefore, a sickle warrior is more likely to find a compatible blood match from a donor of the same race or similar ethnic group.
Over the next few months, the Red Cross Southeastern Pennsylvania and New Jersey regions will be holding several Community of Giving blood drives specifically to help people living with sickle cell disease. The drives are in memory of E. Steven Collins, a legendary Philadelphia radio icon and beloved community leader, who died of a heart attack in 2013.
E. Steven worked as a professional broadcaster for decades with a long tenure at Radio One. He also had numerous areas of civic outreach, including advocating for people with sickle cell disease. He helped bring attention to the cause by supporting community initiatives that increased education and funding.
More than a decade after his death, the Community of Giving blood drives to help those living with sickle cell disease will continue E. Steven’s long legacy of making a difference. The drives will take place from June 12th through September 28th at locations in Southeastern Pennsylvania and New Jersey.
To schedule an appointment to donate blood, visit RedCrossBlood.org.
2024 E. Steven Collins Community of Giving Blood Drives:
Enon Tabernacle Baptist Church
June 29, 9 a.m.-2 p.m.
2800-2900 Cheltenham Ave., Philadelphia
Second Baptist Church of Mount Holly
June 29, 2-7 p.m.
306 Washington St., Mount Holly, N.J.
Epiphany Fellowship Church
July 6, 9 a.m.-2 p.m.
1632 W. Diamond St., Philadelphia
Christian Stronghold Baptist Church
Aug. 8, 8 a.m.-2 p.m.
4701 Lancaster Ave., Philadelphia
Assemblywoman Verlina Reynolds-Jackson
Sept. 6, noon-5 p.m.
431 Pennington Ave., Trenton, N.J.
Office of City Commissioner Omar Sabir
Sept. 24, 10 a.m.-3 p.m.
1400 JFK Blvd., Philadelphia
Lincoln University
Sept. 27, 1-6 p.m.
1570 Baltimore Pike, Lincoln University
Bethlehem Baptist Church
Sept. 28, 9 a.m.-2 p.m.
712 Penllyn Pike, Spring House